News Story
Scarcelli Awarded $2M NIH R01 Grant for Optical Technology to Advance Eye Disease Diagnostics

Fischell Department of Bioengineering Assistant Professor Giuliano Scarcelli was awarded a five-year, $2 million National Institutes of Health (NIH) Research Project Grant (R01) for his efforts to develop an optical technology that could improve diagnosis and management of keratoconus, a progressive eye disease that often begins during a person’s teens or early 20s.
Keratoconus and related eye diseases are a major cause of vision loss in young adults, the primary concern during refractive surgery screening to treat nearsightedness, and the leading indication for corneal transplants in the United States.
Keratoconus causes the cornea – which is normally round – to thin and begin to bulge into a cone-like shape. This cone shape deflects light as it enters the eye on its way to the light-sensitive retina, causing distorted vision. Often, these conditions are triggered by a disruption in the balance between corneal strength and fluid pressure inside the eye, which can naturally occur as the result of a number of ectatic disorders – disorders that weaken the cornea – or as a side effect of refractive surgery.
“While it is critical to identify corneal ectasia [weakening of the cornea] at the earliest time point, current imaging techniques are unable to do that, as they only assess the shape of the cornea and not corneal biomechanics,” Scarcelli said. “This leaves doctors and patients with limited information when diagnosing keratoconus, or when planning surgeries.”
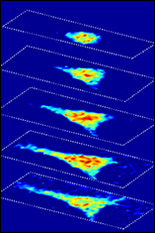
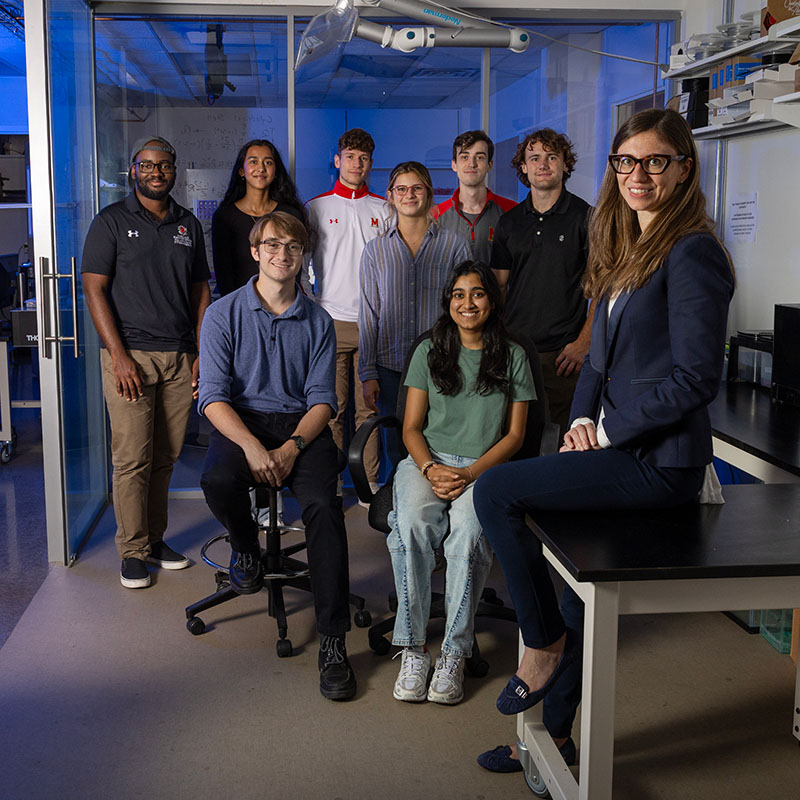
To overcome current corneal screening limitations, Scarcelli and members of his Optics Biotech Lab have applied their own optical technique, known as Brillouin microscopy, to measure corneal stiffness at a high three-dimensional resolution, without contacting or perturbing the eye.
“The overall goals of this research program is to improve diagnosis and management of corneal ecstatic disorders and to improve the safety and outcome of refractive surgery procedures by introducing novel biomechanical profiling of the cornea,” Scarcelli said. “Our central hypothesis is that spatially localized changes in mechanical properties of the cornea are critical drivers of the morphological behavior observed in the clinic.”
With support from the NIH, Scarcelli and clinical collaborator J. Bradley Randleman, MD at University of Southern California will work to validate Brillouin measurements for mechanical evaluation of the cornea, and characterize observed changes in cases of keratoconus. Moving forward, they also hope to determine the mechanical impact of refractive surgery on the cornea.
“This research is significant because elasticity-based metrics will enable us to identify corneal ectasia early on – when treatments are maximally beneficial,” Scarcelli said. “This will also help ensure proper screening of individuals at risk of developing post-operative ectasia who might otherwise undergo LASIK. Ultimately, the knowledge gained from this research is likely to lead to the development of individualized refractive surgery and treatment plans based on the patient’s underlying biomechanical status.”
Earlier this year, Scarcelli was awarded a one-year, $40,000 Shaffer Grant for Innovative Glaucoma Research from the Glaucoma Research Foundation. The grant will support an extension of Scarcelli’s Brillouin microscopy technique to measure stiffness changes in the tissues at the back of the eye in patients with glaucoma. Scarcelli’s hope is that this pilot grant may pave the way towards diagnosing eyes at risk of glaucoma based on the stiffness properties of the sclera and neural tissues, and advance research toward the development of new treatments.
Published March 30, 2018