News Story
BIOE Researchers Publish Study Advancing Probiotic Vesicle Therapy for Inflammatory Bowel Disease
Researchers in the Fischell Department of Bioengineering (BIOE) at the University of Maryland are exploring new research that addresses a major barrier to developing bacterial extracellular vesicle therapies for inflammatory bowel disease. This research, led by BIOE Associate Professor Steven Jay, Robert E. Fischell Distinguished Professor and Director of the Fischell Institute for Biomedical Devices, William E. Bentley, and first author Nicholas Pirolli, was published in Advanced Science and focuses on improving both the effectiveness and manufacturability of probiotic vesicle treatments.

Inflammatory bowel disease affects about 3 million Americans and includes conditions such as Crohn's disease and ulcerative colitis. Many patients do not respond well to existing treatments which often focus on suppressing the immune system rather than addressing underlying gut imbalance and tissue damage. According to their research, bacterial vesicles (BEVs) offer a different approach by directly interacting with the gut environment. Current treatments are ineffective for a significant proportion of people that suffer from IBD and bacterial vesicles have the potential to directly address a major underlying cause of IBD which is an imbalance of normal gut bacteria.
In the study, the research team systematically tested several probiotic strains and found that Lactiplantibacillus plantarum showed the strongest therapeutic promise. The researchers demonstrated that BEVs derived from this strain reduced inflammation and tissue damage in a standard mouse model of colitis. In several experiments, the vesicles performed as well as or better than live probiotic bacteria.
BEVs are naturally released at very low levels which makes them difficult and expensive to manufacture at scale. Jay and Pirolli addressed this challenge by genetically programming L. plantarum to release vesicles at much higher rates. The engineered bacteria produced BEVs dozens of times more efficiently than unmodified strains while maintaining their anti-inflammatory effects.
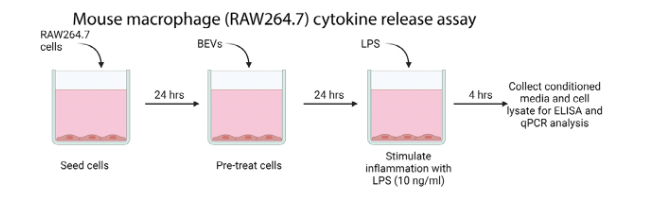
By significantly increasing vesicle yield, the researchers lowered a key cost barrier that has limited the development of vesicle-based therapies and their ability to compete with existing drugs. The team also showed that higher production did not reduce biological activity. In both cell-based experiments and animal studies, the vesicles reduced inflammatory signals and helped preserve the structure of the intestinal lining, indicating that increased production does not compromise therapeutic function.

The study builds on Pirolli’s earlier graduate research in Jay’s lab and supports ongoing efforts to translate the technology toward real-world use. This work also recently led Pirolli securing TEDCO funding to support the development of a platform that enables probiotic bacteria to produce therapeutic vesicles at higher rates without specialized equipment or complex manufacturing processes. The findings reflect a broader effort within BIOE to move microbiome-based therapies closer to clinical application by addressing both biological performance and production challenges.
Looking ahead the team plans to continue refining the technology and exploring how engineered vesicles could be used across a range of inflammatory intestinal diseases. The publication marks an important step in advancing bacterial vesicle therapies from concept to viable therapeutic strategy.
Published January 30, 2026





