News Story
Gemstone Team Investigates New Techniques to Treat Burns

Gemstone Honors Program: Team Tissue
The Fischell Department of Bioengineering (BIOE) and the Robert E. Fischell Institute for Biomedical Devices (REFI) are exploring new ways to develop biocompatible hydrogels for use at the clinical point of care.
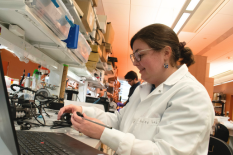
The proposed system is being developed and tested by members of the University of Maryland Gemstone Honors Program who are working to formulate a hydrogel system that encourages wound healing, tissue regeneration, and structural support in order to produce sustainable, biocompatible dermal scaffolds. The group, known as Team Tissue, is comprised of sophomore students studying a broad range of subjects including bioengineering, biochemistry, mechanical engineering, and even history.
According to the American Burn Association, nearly 500,000 burn injuries requiring medical treatment occur each year, and about 40,000 of those require hospitalization.
Today, serious burns are typically treated using allogeneic skin grafts – whereby healthy tissue is harvested from a donor and transplanted to a recipient patient. But, the transplant process – which carries the risk of infection and/or prolonged recovery – relies on a supply of donor tissue. For these reasons, tissue engineers have long sought an alternative through the use of biodegradable scaffolds that mimic organ tissue and promote tissue regrowth and cell proliferation.
In collaboration with REFI, members of Team Tissue are working to fabricate hydrogels that could be used to treat skin and soft tissue excavating wounds after being tailored to individual patients.
Their aim is to cryogenically 3D print vascularized dermal tissue with a hybrid hydrogel composed of collagen, fibrin, and sodium alginate. The process of cryogenic 3D printing involves freezing newly printed bioink - a substance often made of living cells that can be printed into a desired shape – in order to increase the mechanical strength of scaffolds. In order to prevent damage to the cells, Team Tissue, instead, will seed the living cells onto a printed scaffold later in the process. The team believes that optimizing the structural integrity of 3D printed scaffolds and the material components of tissues could pave the way for vascularized channels in engineered tissue.
“While cryogenic temperatures have been used in 3D printing before, researchers are just beginning to explore the possible applications in bioprinting,” said Linnea Warburton, a student in the Department of Mechanical Engineering and a member of Department of Chemical and Biomolecular Engineering Associate Professor Jeffery Klauda’s Molecular & Thermodynamic Modeling Lab. “Our project could demonstrate the benefits of this method for all types of tissue printing, not just for printing dermal tissue.”
Warburton, who plans to one day pursue a graduate degree in bioengineering, serves as Team Tissue’s mentor liaison.
“Additive manufacturing of hydrogels offers an advantage over conventional methods of production because 3D printing enables the hydrogel to have a complex internal structure,” said Dr. Lex Schultheis, REFI faculty member, BIOE Research Professor, and advisor to Team Tissue. “Design of specialized geometry into the hydrogel may optimize drug delivery kinetics. Moreover, the control of the internal structure of the hydrogel allows dosing to be designed into the final product so that each patient, anatomical location or disease state will be treated more effectively than they would with hydrogel medical devices currently available.”
The team is working to construct a cryogenic chamber to control the temperature of the 3D printing process and to alter the solidification of hydrogel scaffold layers. From there, they hope to produce sustainable, biocompatible dermal scaffolds that could one day aid in the treatment of severe burns.
“We hope to build a final product that can be used with many different 3D printers, so that our results can be utilized by researchers doing a variety of types of 3D bioprinting,” said Catherine Liu a biochemistry major working in Department of Biology Assistant Professor Heidi Fisher’s lab. Liu serves as Team Tissue’s financial liaison. “Once we finish building our cryogenic chamber, we will be able to test it with our 3D bioprinter and observe the ways that it alters the printing process. We hope that this novel method of 3D printing will improve quality of 3D printed dermal tissue, and thus have a positive impact on patients in need of skin grafts.”
The full list of Team Tissue members is as follows: Yahya Cheema (BIOE; History minor), Kunal Dharmadhikari (BIOE; Computer Science minor); Michael Hildreth (BIOE and English Language and Literature double-major); Neal Kewalramani (BIOE and Mathematics double-major); Catherine Liu (Biochemistry); Alexi Rodriguez (BIOE; Mathematics minor); Danielle Sidelnikov (Neurobiology and Physiology and History double-major); Pavan Vemulakonda (BIOE; Philosophy minor); and Linnea Warburton (Mechanical Engineering).
Published May 15, 2018