News Story
BIOE Capstone Competition Highlights 24 Novel Projects
On Monday, May 2, the Fischell Department of Bioengineering (BIOE) Senior Capstone class presented 24 novel concepts in the first in-person competition in A. James Clark Hall since 2019. Projects ranged from an augmented reality application for performing lunbar punctures, to an automated cardiac compression device, to a biometric-based unique patient identifier.
A total of 119 BIOE students pitched their concepts to judges from the BIOE Advisory Board, as well as to faculty, industry representatives, mentors, and friends and family who attended the event. The four Capstone groups that advanced to the finals presented their projects to all in attendance in the Zupnik Forum.
This year's panel of judges featured:
-
The Bioengineering Graduate Student Society
-
Students who voted in the Students' Choice Award category
The Fischell Department of Bioengineering receives support for its Capstone Design competition from the Fischell Family, the University of Maryland MPowering the State Strategic Partnership, and industrial sponsor BD. Additionally, Capstone students often receive mentorship support from industry representatives and/or clinicians, including investigators from the University of Maryland School of Medicine, Children's National Health Center, the U.S. Food and Drug Administration, the University of Maryland Robert E. Fischell Institute for Biomedical Devices.
 Team 1: Biometric-Based Unique Patient Identifier
Team 1: Biometric-Based Unique Patient Identifier
Elizabeth Kinnard, Kaitlyn Kordela, Gabrielle Lavarias, Yasmine Pierre, Camryn Stanley
Advisors: Dr. Alisa Clyne, and Dr. Naresh Menon (ChromoLogic)
For an estimated 11% of U.S. voting-age citizens and many more U.S. residents that do not have valid government-issued identification, acquiring inexpensive and adequate insurance and healthcare is difficult, if not impossible, creating limited acess for the underrepresented minority groups (Black and Latino families) that make up the majority of this statistic. The use of biometrics to secure and unlock one’s medical records have the potential to be a solution since biometrics such as fingerprints and irises are unique to each person and hardly change over a person’s lifetime. These features may be attractive for both patients and providers due to security, decreased waiting room times, and increased accessibility. Thus, the team modified Chromologic Inc.’s Biometric Authentication and Identification Device (BAID) to fit consumer needs by aiming to decrease enrollment times, increase public acceptance of BAID, and make the design ADA/DDA compliant. Initial component testing revealed that the iris scanner contributed to most of the variation in enrollment time; thus, focus was placed on redesigning the iris scanner. Modifications to the iris scanner include a shorter scanning distance, removal of obstructive components from the original BAID design, and the addition of a gooseneck attachment for angle adjustment. Other modifications to the general design of BAID include a mobile and height-adjustable base, compliance for a tablet with a gooseneck attachment, handprint mold for intuitive fingerprint placement, and a more accessible app redesign (options for different languages, text-to-speech, etc.). The redesign showed decreased overall and iris scanning enrollment times reaching significance (p=0.055 and p=0.076 respectively). Though the design fulfilled two of the goals, further testing with a greater sample size as well as gathering acceptance data via a distributed survey would more accurately describe the success of the redesign and potential for commercial use. Future steps for this project include integration of EPIC, greater administrative control of the software, and simultaneous biometric scanning. The team hopes that the eventual implementation of this design in healthcare would allow disadvantaged populations to receive appropriate healthcare regardless of documented status. However, the team also acknowledges that sharing one's biometrics may sound invasive which the team mitigated by having this scanning procedure be HIPAA compliant and using FBI-approved scanners.
Team 2: Remote Monitoring of Forelimb Rehabilitation
Dalia Kassas, Danielle Cornwell, Davis Kelley, Sharvari Puri, Erfan Jabari
Advisors: Dr. Paola Pergami and Dr. Li-Qun Zhang
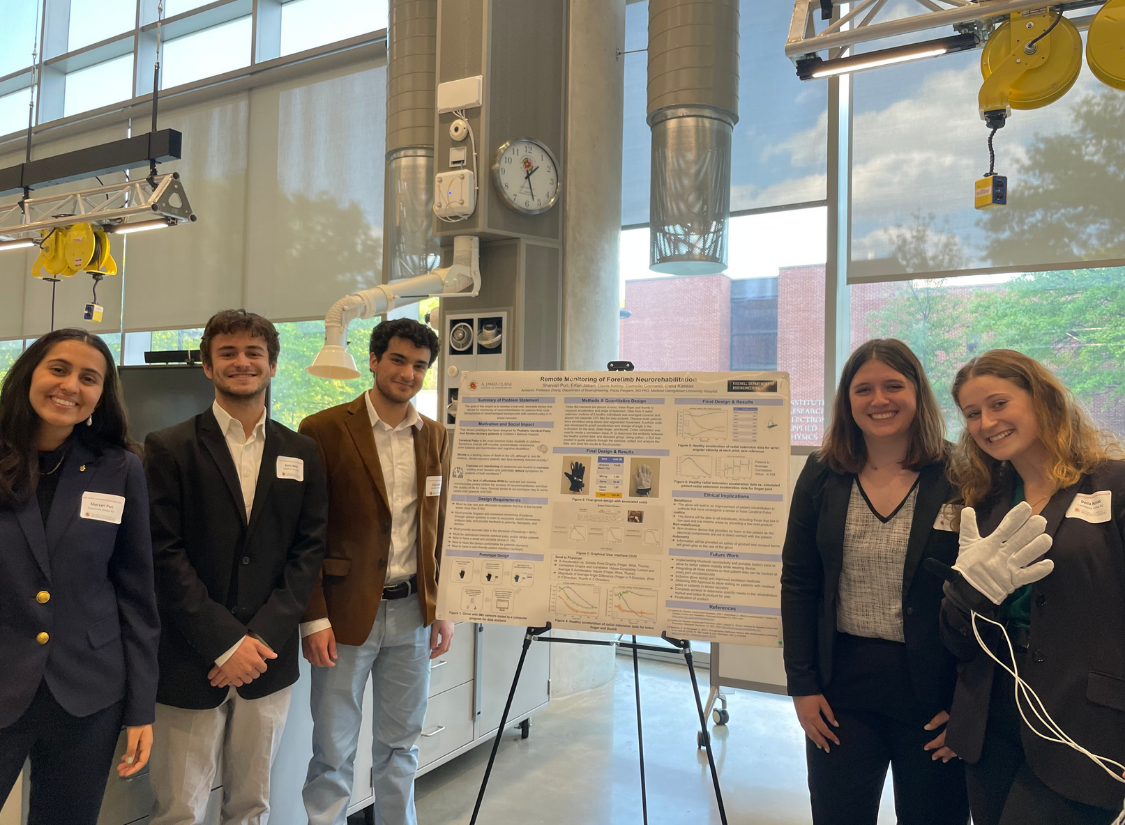
BEST ABSTRACT
The inability of cerebral palsy and/or stroke patients in low income and rural areas to consistently access specialized facilities for monitoring of neurorehabilitation is a serious detriment to the recovery process. As such, bridging the gap between these patients and much needed monitoring is necessary to enhance the effectiveness of the treatment they receive. Current systems for remote neurorehabilitation monitoring are cost-prohibitive for many affected patients. Additionally, many of these devices target a very limited range of motion, further limiting their clinical utility. We sought to develop an accessible device for at home asynchronous use that monitors neurorehabilitation by tracking the recovery of function in boththe hand and wrist of cerebral palsy and/or stroke patients. Specifically, we aimed for our deviceto be low-cost, user-friendly, and easy to understand for patients from underprivileged areas with low health literacy. In this effort, we designed a glove that assesses radial extension of the wrist, extension of the thumb, and extension of the index finger.The device utilizes Arduino Nano 33 BLEs with onboard Inertial Measurement Units (IMUs) mated to a Python program to extract acceleration and change in angle of extension of the wrist, thumb, and index finger during simple hand and wrist exercises. This program successfully performs a statistical comparison of recorded measurement to healthy baseline data to track hand and wrist motor function capacity in patients. A user-friendly Graphical User Interface (GUI) was also developed using Python to allow patients to operate the device, view results, and share results with a physician. Ultimately,we believe our device provides an essential platform for cerebral palsy and/or stroke patients from low-income or rural backgrounds to access care for forelimb rehabilitation.
Ezra Cho, Brian Huang, Hyojin Kuan, Nick Staten, Sam Yee
Advisors: Dr. Cedric Yu and Dr. Hubert Montas
ADVISORY BOARD AWARD FOR TRANSLATIONAL DESIGN 
To address the need for better early-stage breast cancer treatment, Dr. Cedric Yu of the University of Maryland Medical Center invented the GammaPod, a noninvasive, first-of-its-kind stereotactic body radiation therapy (SBRT) device to treat breast tumors while minimally impacting the surrounding healthy tissue. Compared to conventional surgery and radiation treatments, the GammaPod effectively reduces the breast cancer treatment timeline from 4-6 weeks to 1-5 days. In order to stereotactically target tumors, the patient’s breast must first be immobilized by vacuum-sealing the breast into a patented GammaPod breast cup ranging from 30 different sizes. Fitting the patients for these cups currently involves manual trial-and-error for clinicians, resulting in an average of 2-3 discarded cups per patient, increased treatment time, and substantial patient discomfort from failed fitting attempts. In order to address these issues, our Capstone group designed a no-contact imaging system to quickly and accurately determine the appropriate cup size to use while minimizing patient discomfort. Our prototype, which was validated on isolated silicone breast forms of various sizes, consists of three components: a chassis, an imaging system, and a software system. The chassis is a 2’x2’x5’ structure that houses two cameras to image the targeted breast. The imaging system consists of two Intel RealSense D435i RGBD cameras, which are connected to a Raspberry Pi processing unit. Lastly, the software system converts the obtained depth images into a merged point cloud to calculate the target breast’s volume and base diameter consistently within 5 minutes and within a 5% error of the uncalibrated average. The ethical implications of this prototype include minimization of suffering for the patient as well as patient privacy protection. The design mitigates patient suffering by reducing the physical discomfort associated with time-consuming misfittings, while the imaging and software systems maintain patient privacy by deleting the images after the fitting process is completed. Future work on this device would involve optimizing and calibrating the software system to more accurately determine breast measurements, as well as validating the system on a manikin and ultimately human patients.
Team 4: Neonatal Volume-Controlled Attachment for Bag Mask Ventilator
Ashley Hawkins, John Osborne, Vené Richardson-Powell, Matthew Graham, Sarayu Iyer
Advisors: Dr. Catherine K. Kuo and Dr. John Idso
BEST POSTER 
Ten percent of neonates require medical intervention to initiate breathing at birth. The most common method of resuscitation in the delivery room is bag valve mask (BVM) ventilation, which allows physicians to control pressure effectively, but not volume. A common complication is an iatrogenic pneumothorax - the result of excessive tidal volumes of air being ventilated into the neonate’s lungs and pleural cavity. The limited ability of a physician to control the tidal volume increases the risk of barotrauma and pneumothorax in all cases of bag mask ventilation; moreover, as little as 3mL of excess tidal volume ventilated into a neonate's lungs can cause a pneumothorax. Herein, we designed a syringe-based attachment to a standard BVM with the goal of delivering 3-30 mL of air to neonates while preserving the common BVM ventilation procedure. The device attaches downstream of the neonate mask and pressure control valves, but upstream of the self inflating bag. When the self inflating bag is compressed by the physician, the pressure generated inside the bag acts on the plunger in the syringe-attachment, depressing it. Adjustable stops were placed every 5mL along the main syringe body to ensure the plunger only depresses to a fixed volume chosen by the physician. Furthermore, the plunger is loaded with a tension spring that allows the plunger to return to its resting position when the self inflating bag is relaxed by the physician. Initial 3D printed prototype results showed an average delivery of 3.2 ± 1.1 mL of air for a desired 3mL and an average of 7.8 ± 2.9 mL for a desired 30mL of air. Our future work aims to increase our accuracy by ensuring airtightness, increasing the 3D print resolution, and finding a new material to print with a lower coefficient of friction. The volume-controlled attachment is compatible with the current single-use manufactured BVM resuscitation device. Thus, it can be utilized throughout U.S. medical facilities and as well as countries with similar medical standards. We recognize that the single-use nature is a common U.S medical device standard but would not prove useful in countries with low financial resources. Additionally, single-use design would have a negative environmental impact. These concerns are important and are considered when innovating our future design. Nevertheless, the positive impact of the device could save a number of neonates from future complications caused by a pneumothorax.
Team 5: Biomechanical Analysis of Proximal Femoral Varus Osteotomy Fixation
Dina Eloseily, Michael He, Lauren Losin, Neelesh Mupparapu, Grace Powers
Advisors: Dr. Sean Tabaie and Dr. Martha Wang
 In pediatric Cerebral Palsy (CP) patients, hip dysplasia may develop due to spasticity. This often requires a corrective gap osteotomy of the proximal end of the femur to varus (
In pediatric Cerebral Palsy (CP) patients, hip dysplasia may develop due to spasticity. This often requires a corrective gap osteotomy of the proximal end of the femur to varus (
Team 6: Development of a Multi-Sample Endomyocardial Bioptome Designed to Reduce Vascular Trauma
Annette Bernier, Sarah Browning, Anna Parrish, Nikita Singh
Advisors: Dr. Mukta Srivastava and Dr. Katharina Maisel
MPOWER AWARD 
Endomyocardial biopsies conducted with the standard bioptome for surveillance of post-orthotopic heart transplant rejection and native heart failure come with risk of cardiac trauma. For pathological analysis of organ rejection, 4-6 tissue samples from the interventricular septum are needed. This area is accessed via the right ventricle, after passing the bioptome through the tricuspid valve. The current biopsy method requires withdrawing and re-advancing the bioptome device in between the collection of each sample. Each pass done by the clinician to the interventricular septum can cause damage to the chordae tendineae that attach the tricuspid valve to the walls of the heart, potentially leading to future corrective surgery if damage is significant. The risk for cardiovascular trauma is exacerbated by the high frequency of endomyocardial biopsies that transplant patients must have, with patients having this procedure regularly for several years post-transplant. To address this challenge, our project’s primary objective is to design a multi-sample bioptome for use in endomyocardial biopsies that only requires a single insertion into the patient. Alongside of this, our design will reduce patient complications by minimizing trauma caused by the device and reducing overall procedure length. Our proposed device completes the objective through the redesign of the standard device to include a storage component attached to the pincer head that will allow for 4-6 samples (1-2 mm each) to be collected at one time before removing the bioptome from the patient. Tissue samples will be cut off and enclosed within the double action pincer head where syringe-like suction will be applied by the clinician to pull the tissue samples into the chamber. Our prototyping results focused on the novel aspect of our device: the sample chamber and syringe mechanism. A to-scale handle mechanism coupled with a 2x scale chamber and sample collection shows proof of concept for our current device while providing looks-like and works-like sections of the device. Our device will improve the efficiency of the overall biopsy procedure and mitigate the risk of cardiovascular trauma in patients typically caused by the repeated sampling needed from the current device.
Team 7: A Mechanical Dilator to Optimize Vascular Access in Critical Care
Thilinie Kuruppu, Yusuf Mastoor, Lydia Runnals, Sagar Matharu, Alex Ramos, Joseph Rabin
Advisors: Dr. Steven Jay and Dr. Joseph Rabin
STUDENT'S CHOICE 
Percutaneous vascular access is a crucial and required step for initiating severe respiratory failure patients on extracorporeal membrane oxygenation (ECMO). ECMO is a bridge treatment which provides mechanical cardiopulmonary support to critically ill patients in an intensive care unit (ICU) setting. Vascular access is established using ultrasound guided percutaneous insertion of a guide wire. This access is expanded to accommodate an ECMO cannula using a series of dilators of increasing size that are inserted and removed over the guidewire. Complications can occur during this such as bending or complete removal of the guidewire. These often result in clinicians having to restart the entire procedure, ultimately costing the patient more time. This project, therefore, aims to develop and design a mechanical vascular dilator which will be able to expand and provide cannula access faster and more effectively as compared to the standard of care. To address this, we developed and tested a balloon-based vascular dilator composed of polydimethylsiloxane (PDMS) and metal leaflets. Our larger than scale model was able to expand up to 23% of its initial diameter without any folding or compression prior to expansion. The device will also be used to dilate an animal vessel in an ex vivo ECMO circuit. In order to adapt this prototype for clinical use, the device will be manufactured at a smaller scale and incorporated into currently used vascular cannulas as an attachment. With the development of this device, initiating ECMO for patients will be more streamlined, quicker, and efficient for clinicians and providers.
Team 8: Tele-Neurorehabilitation After Stroke: Validation of LiDAR for Human Pose Estimation
Maximillian Berenschot, Sabrina De Nicola, Lauren Hoorens Van Heyningen, Noriana Jakopin, Jennifer Song
Advisors: Dr. Kim Stroka, Dr. Richard Macko and Dr. Charlene Hafer-Macko 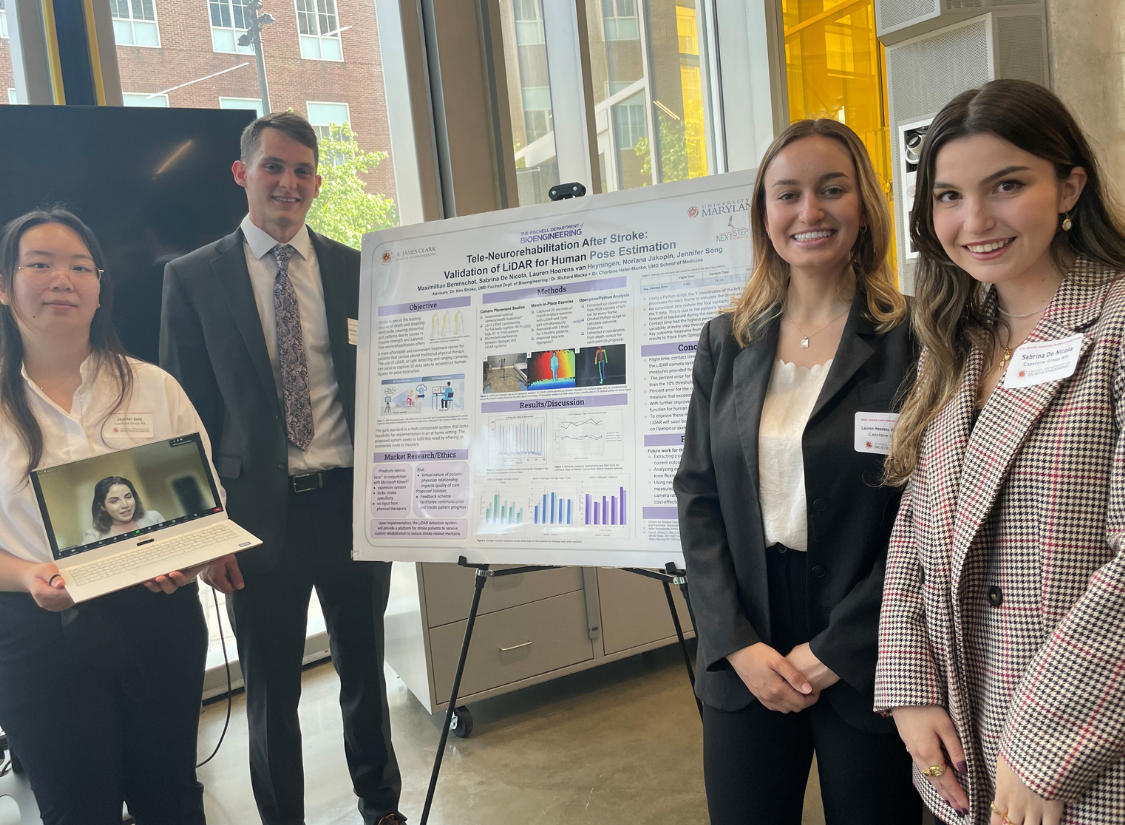
Stroke is the second leading cause of death worldwide, claiming over 130,000 lives in the United States alone each year. Survivors of stroke often suffer from a multitude of impairments, such as decrease in muscle strength, inability to balance, and an overall loss in mobility. These issues are typically treated through physical therapy in the presence of a medical professional; however, this is not accessible to many stroke patients due to high costs, difficulties with traveling, and additional restrictions as a result of the ongoing COVID-19 pandemic. A possible solution may lie in a digital neuro-telerehabilitation program that provides physical therapists with a platform to create personalized therapeutic programs for stroke patients. LiDAR, or light detecting and ranging cameras, record three dimensional data which is then used to construct a human figure. LiDAR will be validated against the gold standard Optogait system as a potential alternative for motion capture to perform movement analysis. By recording the march-in-place exercise with the LiDAR camera system and processing the data with Openpose software, the X & Y coordinates of 25 key skeletal points were generated for every frame. The coordinates were then processed through a Python script to precisely track movements and calculate cadence, flight time, and contact time of the foot. The percent error between the LiDAR system and the Optogait system was 9.9%, 19.3%, and 8.9% for flight time, contact time, and cadence, respectively. Results show that the 2-dimensional data alone is slightly outside of the acceptable error when compared to a validated system. This points to the importance of mapping the depth data to the X & Y coordinates to improve accuracy, which is in progress and is the immediate next step. Though the telemedicine platform is an external system, there are several risks to consider. It is imperative that the virtual nature of the patient-physician relationship does not diminish the quality of care that the patient receives. To solve this, future steps will focus on the development of a feedback scheme to facilitate communication and track the patient’s progress. In terms of privacy, there will be a secure connection that can only be accessed by the two consenting parties. If implemented, the LiDAR system will positively impact the lives of stroke patients by offering them an accessible route to recovery.
Team 9: Rapid Automated Cell Expansion and HyperspectraImaging Monitoring for Improving the Production of Cell Therapy Drugs
Jess Conway, Anya Filatova, Amy Musser, Anthony Neri, Yiding Yuan
Advisors: Dr. Maurizio Cattaneo, Dr. Yang Tao, Anjana Heva, Chiao-Yi Wang, Callie Weber, Dr. William Bentley, Dr. Chen-Yu Tsao 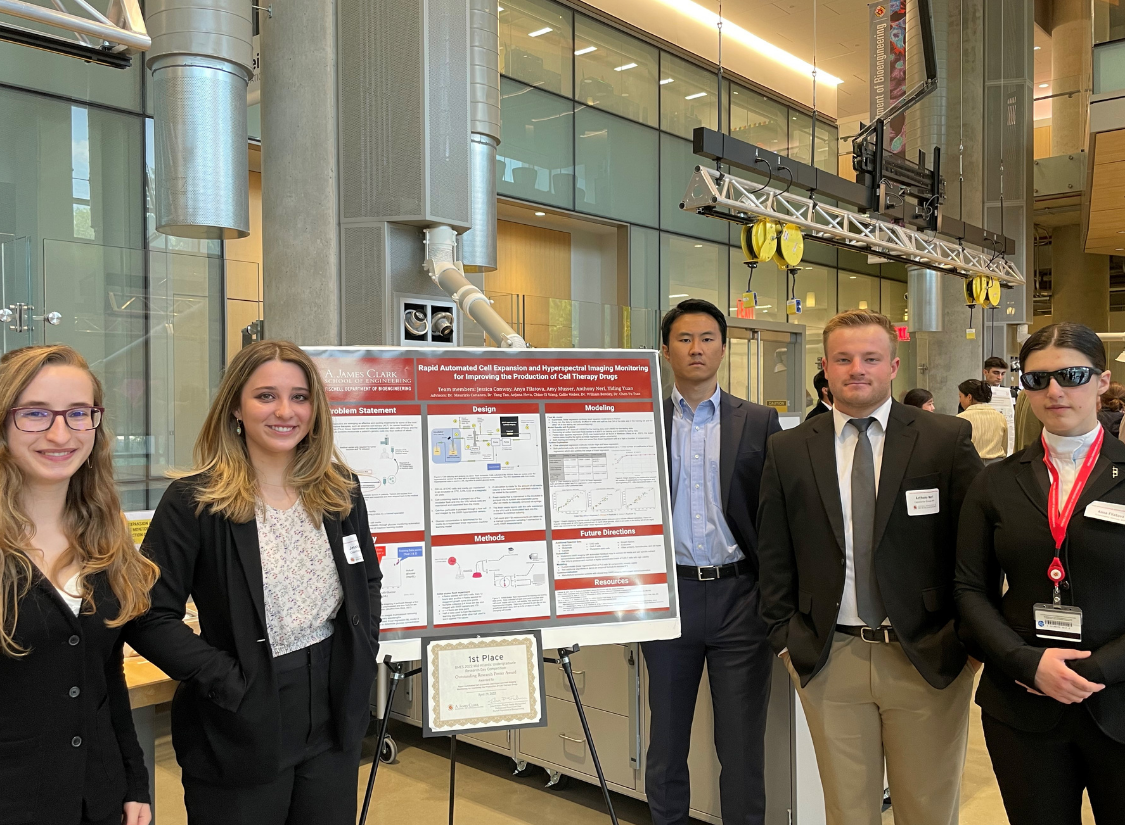
Personalized, cell-based therapeutics are emerging as effective and exciting treatments for some of the most severe diseases. These innovative therapies, such as adoptive cell therapy (ACT) for cancer treatment by tumor-infiltrating T-lymphocytes (TILs), tissue regeneration via induced pluripotent stem cells (iPSCs), and the use of cell-produced therapeutic proteins incorporate a patient’s genetic code into their method of attack. Industrial cell expansion via a bioreactor is a crucial step in the production of cell-based therapeutics. Constraints to this process include the transfer and isolation of cell samples to a separate facility and manual intervention with highly invasive cell monitoring probes by a trained specialist. This increases the production time, cost, and risk of contamination, raising the price per patient for these potentially life-saving therapies. The goal of this project is to increase the efficacy and therefore the availability and affordability of cell-based therapeutics by automating glucose concentration monitoring in bioreactor cell cultures. Our team combined a short-wave infrared (SWIR) hyperspectral camera with a flask bioreactor and a deep learning algorithm to non-invasively determine glucose concentration in the media. CHO cells were seeded and grown in a reusable spinner flask and then were pumped by a magnetic drive pump through an Artemis Biosystem’s VHU (viral harvesting unit), where the cells are maintained allowing the perfusate to flow through a flow cell and imaged by the hyperspectral camera and pumped back into the flask bioreactor. The hyperspectral data was fed into a supervised linear regression (ordinary least squares/OLS) ML model in Python that achieved a R2 score of 0.92062 for training data and 0.89065 for testing data. Removing an outlier at 9.45 mg/dL improved these values to 0.95978 and 0.94009 for training and testing data respectively. PLS regression achieved a R2 score of 0.95863 for training data and 0.94848 for testing data, which is about the same performance as OLS. Based on these models additional media is supplied via a peristaltic pump to achieve the determined desired glucose level. Future applications of this process can enable the industrial culture of multiple cell types and imaging via low-cost infrared spectroscopy devices, further increasing the availability of cell-based therapeutics. This non-invasive method may also be applied to other parameters of a bioreactor that need to be monitored as well, reducing the amount of attention that the cell expansion phase requires. By reducing contamination risk and increasing the efficiency of bioreactor cell expansion, personalized therapies have the potential to become a more feasible method of fighting various diseases.
Team 10: Infant transanal rectal suction biopsy device with external stabilization
Noemi Gonzalez-Martinez, Varunaa Hemanth, Anish Kakarla, Yaniv Kovich, and Tia Puskar
Advisors: Dr. Helim Aranda-Espinoza and Dr. Louis Marmon 
Hirschsprung disease is a congenital condition where missing nerve cells in the large intestine cause issues passing stool. The lack of nerve cells in the muscles of the colon reduces stimulation in the gut which helps stool move through the colon and can cause bowel blockages. In order to diagnose the disease, an infant transanal rectal suction biopsy device is “blindly” inserting the instrument into the infant’s rectum. If the results of the biopsy diagnose the infant with Hirschsprung disease, then surgery will be required to bypass the part of the large intestines lacking nerves. Currently, the RBI2 Suction Rectal Biopsy System is what is used to conduct infant rectal biopsies but when clinicians use this device is it difficult for them to stabilize the probe. Proper biopsy location is critical to ensure that the target tissue is obtained and a proper diagnosis can be made. The current method lacks a reliable way to visualize where the piece of tissue needs to be taken, relying on a physician's vision alone. An accident could result in a tissue biopsy in the wrong adjacent areas such as the skin, anoderm, or pectinate area. In the past, incorrect biopsies have led to rectal hemorrhages and, in severe cases, death from gangrene of the buttocks. The product we are designing is an external stabilization disk for use in conjunction with an infant transanal rectal suction biopsy device to help the clinician visualize how far up the rectum the probe is. This product would be an add-on to the current biopsy device. The device should be able to move up and down in order to change the desired length entered into the rectum. Initial prototype will be designed by printing the clasp out of Polylactic acid (PLA) filament using a 3D printer, would be the best method. Rubber inserts will also be purchased to complete the prototype. The testing of the assembled device includes stabilization and mobility of the add-on product. Stabilization testing showed that as the force applied increased the displacement increased as well. From our criteria and the results we decided on making the prototype 2.5 cm in length. Using a two sample t-test, the results from the grid testing showed that there is a significant difference in stabilization when the disk is added to the probe compared to the probe itself. Our device has a positive ethical device because it benefits the infant and the clinician by giving more accurate diagnostic results.
Team 11: Deep Learning for Automated Expert-Level Diagnosis of Sports Injuries on Knee MRI
Anagha Rama Varma, Keyona Curry, Anna Fraser, Janam Shankar
Advisors: Dr. Xioaming He and Dr. Paul Yi 
ACL tears account for approximately 50% of all knee injuries (Joseph, 2013). The diagnosis of ACL tears often relies on the assessment of an MRI image of the knee by an experienced radiologist. However, where such a provider may be unavailable, diagnosis may be delayed, which increases the potential for further complications. In order to address this disparity, we have developed a 2D convolutional neural network deep learning model which can diagnose the presence of an ACL tear from an MRI image input and can predict the presence of an ACL tear with 82.7% accuracy. This model was based on the Stanford MRNet model, which was modified to exclusively perform ACL tear diagnosis and trained on an expanded data set of 1947 knee MRI images. We have additionally developed a user interface to facilitate ease of use in a clinical care setting. The availability of this technology will increase access to accurate diagnosis for all communities and can also act as a method of diagnosis confirmation for clinicians, increasing the likelihood of accurate and prompt diagnosis of ACL tears and reducing the risk for complications.
Team 12: Designing a Strain Gauge for Laparoscopic Surgery
Lauren Becker, Justin Ciemian, Sarah Covert, Scott Fan-Loh, Keren Sneh
Advisors: Dr. Brian Blair and Dr. Louis Marmon 
Laparoscopic surgery is a type of minimally invasive surgery, specifically for abdominal procedures, in which long-handled instruments are inserted into small incisions in the abdomen so surgery can be performed without having to fully open the abdomen. Laparoscopic approaches have been shown to greatly reduce surgical complications and recovery time. However, due to the significant length of the instrument, surgeons experience a lack of tactile feedback during surgery. This absence of tactile feedback makes it difficult for surgeons to assess how much force is being applied to tissues or when suturing, which can lead to dangerous mistakes. The objective of our project is to create a device that reliably measures the force applied by the jaws of a laparoscopic instrument and displays this force to the surgeon. The successful implementation of this project would positively impact surgeons and their patients. Surgeons would be more confident during their procedures, resulting in fewer mistakes being made. In order to achieve our objectives, we chose to place our strain gauges on the internal shaft of the laparoscopic grasper where they will measure the deformation of the bar when the jaws are opened and closed. Our 3D printed prototype did not deform enough to be detected by the strain gauges, however our design using the internal shaft of the original laparoscope had successful results. Using Arduino software, we were able to measure the change in voltage between the Wheatstone bridge when the internal shaft experienced bending.
Team 13: Developing an Automated Cardiac Compression Device
Katelyn Kunert, Esther Katz, James Latoff, Nicolas Sanchez Manni, and Christina Ternovskaia
Advisors: Dr. Tao Lowe and Dr. Ron E. Samet 
Chest compressions and automated external defibrillators (AEDs) are established methods for treating cardiac arrest when the chest is closed. During cardiac surgery or emergency thoracotomy when the chest is open, if a patient’s heart stops it must be massaged manually which does not allow for the necessary pressure buildup to restart blood flow and is difficult to do correctly and effectively. We prototyped an automated cardiac compression sleeve that displaces a clinical relevant amount of fluid per beat, can be operated at 100 bpm, and assists in defibrillation with currently available devices. Our device utilizes three pneumatically controlled Mckibben actuators and solenoid valves controlled by an Arduino to compress the heart and restore cardiac output. Our sleeve displaced ~60 ml of fluid per beat without slipping when tested over 30 seconds. Defibrillation paddles can be placed underneath the polyester sleeve to help hold the paddles in place against the heart. The sleeve takes ~12 seconds to put onto the heart and can be taken off easily in less time due to velcro and elastic that make the sleeve flexible and suitable for different sized hearts. Overall, our prototype demonstrates the ability to displace a clinically relevant amount of fluid on a model heart and has the potential to move towards an animal model in the future.
Team 14: Replicating the Force and Dexterity of a Human Hand in a Cost-Effective Robotic End-Effector
Emma Stevens, Anya Skae, Shruthi Krishnamurthy, Jonathan Montenegro, Benjamin Wu
Advisors: Dr. Yang Tao
The export of crabs, specifically blue crabs, are one of the major exports of the East Coast, especially Maryland. There is a large probability for workers to obtain allergies to the product as well as increased difficulty obtaining work visas as a result of the COVID-19 pandemic thus the turnover of workers is increased as opposed to other industries and overall less workers in the industry. With this in mind, the project goal was to create a cost effective, end-effector device that aids in manipulating crabs robotically to mitigate lack of workers, and increase worker safety and health in the East Coast Crab Manufacturing Industry. In order to accurately supplement a human hand, the dexterity and force that it provides simultaneously was aimed for. The solution targeted the dexterity portion of that goal by attempting to articulate all of the joints in the finger and thumb, since many models, especially those that used our chosen mechanism of gears, leave the DIP (distal interphalangeal) joint in the finger and the PIP (proximal interphalangeal) joint in the thumb unarticulated. This would give greater control over the digits’ grasping motion. The results of this approach were unfortunately not obtained, however the force that could be generated by the chosen motor using a single finger of the same length and proportions exceeded that which is required to manipulate even the largest of blue crabs. The ethical impact of this project would allow workers in the crab extraction industry to stay healthy so they can continue to work in the industry more than they were able to prior, with healthier working hours and overall environment. That being said, there is a possibility that automation would become advanced enough to replace workers, which may be an ethical concern for the company to address.
Team 15: Forming a Solid Separation Barrier in Microcentrifuge Plasma Separating Tubes Using Polystyrene Beads
Riley Donnelly, Christina Kilby, Morgan Pettebone, Ari Sporkin, Lexi Wittstadt
Advisors: Dr. Kishore Bokka, Dr. Arun Nair, Dr. Angela Jones 
Plasma is necessary to diagnose diseases such as HIV, hepatitis, parasitic disease, thrombotic thrombocytopenic purpura (TTP), and Von Willebrand disease as well as clotting disorders. Capillary samples are collected in a microcentrifuge plasma separating tubes (PSTs) which has a polymeric separator gel. Under centrifugation, the plasma is separated from the cellular components of the blood because the separator gel has a density between blood cells and plasma, which creates a barrier between the components. To collect the plasma layer for testing,an automated probe is lowered into the tube, stops at a set distance above the gel, and aspirates the sample. However, the probe does not lower to the gel layer because it will be damaged if the gel is aspirated. As a result, a fraction of plasma above the gel layer is not collected. This fraction is referred to as the “buffer zone,” which can range from one to three millimeters depending on the sample size and hematocrit levels. Therefore, more blood is collected than used for testing due to collection inefficiency. This problem is magnified when collecting capillary blood samples due to the small volume. The goal is to aspirate all the plasma available in a sample. This project designed a solution using polymeric beads that creates a solid barrier separating the plasma from the other components. This eliminates the buffer zone by allowing the probe to make contact with the solid barrier and aspirate all the plasma available. Thereby maximizing plasma collection per sample without the risk of the probe damage. The prototype design used polystyrene beads with a density between the hydrophobic gel and the plasma layer, arranged in both monolayer (eight beads) and bilayer (sixteen beads) orientations. The beads,gel, and blood were centrifuged and the plasma was collected post centrifugation. Prototype testing displayed instrumental results. Hemolysis levels in plasma were not affected by the addition of beads, there was no significant difference in plasma collection between the control and experimental groups, and the bead barrier did not require a buffer zone. These results indicate that this project demonstrated key successes in solving the underlying healthcare problem. The prototype is compatible with existing collection devices. This project has the potential to improve diagnostics and outcomes for those with severe blood and clotting disorders as well as anyone who requires frequent plasma testing since greater collection efficiency reduces the number of samples required . This project also improves provider resource management, as it requires fewer collection tubes per patient. This in turn reduces the environmental footprint of plasma testing by decreasing the amount of plastic used by healthcare providers.
Team 16: Eye Model for the Verification of Erythrocyte Mediated Angiography
Kaitlyn Albus, Decklan Fischer, Lucas Garcia-O’Donnell, Nicole Miranda, Madelyn Morse
Advisors: Dr. Osamah Saeedi and Dr. Angela Jones
An earlier and more accurate diagnosis can lead to faster and higher chances of successful treatment for patients who suffer from eye issues that can cause blindness such as glaucoma, age-related macular degeneration, and diabetic retinopathy. Early detection and diagnosis of these diseases can lead to overall better treatment and outcome. We aim to improve the current method of diagnosis by creating a simplified and accurate phantom eye model. One way to diagnose such diseases includes measuring ocular blood flow and currently, the best method for this is erythrocyte mediated angiography (EMA). Essentially, EMA calculates the blood velocity in the eye capillaries by using a Heidelberg Retinal Tomography (HRT) imaging device to track the movement of fluorescently labeled blood cells. While this methodology is effective, EMA encompasses certain assumptions about the eye anatomy that are not necessarily correct. Ultimately, eye length and len’s power can vary on a patient to patient basis depending on the size of the lens and location of the eye capillary beds. Since the effectiveness of EMA isreliant on how well the eye can be imaged and this method does not take either of anatomical factors into consideration, it is not known for sure if the overall procedure is wholly accurate.Therefore, the assumptions that we aim to improve upon with this project are overall eye length and the relative power of the eye’s lens and cornea. Through intensive literature and patent review, we designed our phantom eye that will improve the reliability of blood flow measurements by having controllable axial eye length and magnification power. Our design incorporates three changeable focal lenses (15, 18, 20 mm) and three axial length notches (18, 22, 26 mm) that account for the ocular variables. In order to mimic erythrocyte flow, we adhered fluorescent microspheres on a conveyor belt system powered by a DC motor that moves at a rate comparable to blood cell velocity in the eye. The use of our phantom eye is to verify and potentially calibrate ocular imaging devices like the HRT used in EMA based on a patient's individual eye parameters. Our results suggest that longer axial distances may affect the HRT’s ability to track blood velocity accurately and that the HRT may also have difficulty in recording accurate velocities from patients with lower lens focal lengths. Our device will benefit patients with eye diseases causing blindness because our phantom eye will improve the accuracy of the HRT results and diagnoses. However, our device could also be improved by adding more values of axial lengths and focal lengths to be more accessible. Overall, this model will provide more accurate measurements of ocular blood flow. This allows for significant advancements in the ophthalmology field and can improve patient well-being through earlier and more accurate diagnoses.
Team 17: A Self-Sealing, Minimally Invasive Cannula for Assisted Circulation
Alonso Arribas, Katarina Koziol, Katherine May, Erik Vaughan, and Julia Zhiteneva
Advisors: Dr. Zhongjun Wu and Dr. John Fisher
THIRD PLACE 
Extracorporeal membrane oxygenation (ECMO) provides mechanical assistance to patients lacking functional lungs or a heart due to cardiovascular disease or acute trauma. ECMO is highly invasive and trauma-inducing, leaving patients susceptible to bleeding, vascular complications, infection, and ischemia. Often employing two single-lumen cannulas, cannula insertion into the vasculature heightens these risks. While there are dual-lumen cannulas on the market, eliminating the need for two, the aforementioned issues are exacerbated by the minimal distance between infusion and drainage ports. Our solution was to create a singular dual lumen cannula (DLC) with nitinol leaflets for stabilization and a one-way pressure stable valve for self-sealing. This device will minimize invasion and trauma for patients by completely avoiding the vasculature, based on a patent of UMSOM’s Dr. Zhongjun Wu. Our initial prototyping with a PDMS phantom heart and an ex vivo porcine heart demonstrated the need to modify the cannula material to be more sturdy, shorten the length of both the double umbrella body and self-sealing leaflets, and modify the silicone valve design for functionality. This minimally invasive, self-sealing DLC will increase accessibility by reducing surgical duration and complexity, promoting quicker recovery and therefore decreasing hospital-stay costs. Additionally, we hope to improve patient trust in healthcare by this reduction of surgical risks and complications.
Team 18: Point-of-use reusable respirator decontamination system
Yasmin Azem, Chris Hannon, Emily Leo, Hiya Sawney, and Emma Schaefer
Advisors: Dr. Stella Hines and Dr. Gregg Duncan 
Especially in the midst of the ongoing pandemic, there is an increased need for an efficient and effective way for healthcare workers to disinfect their reusable respirators between patient visits. It is necessary for healthcare workers to protect themselves and their patients by thoroughly disinfecting their respirator, if not between seeing patients, at least at the end of their shift. This is also vital for the well-being of healthcare workers as, over the course of a day, a number of potentially dangerous particulates could gather in the respirator, making it less effective. However, there is no optimized procedure or product to disinfect respirators to an accepted standard. Currently, the accepted practice for decontaminating reusable respirators between patients is to manually wipe with disinfectant wipes, used often in tandem with centralized decontamination conducted approximately everyday. The current protocol of wiping down respirators with disinfecting wipes is lacking as it does not destroy all potentially infectious particulates and often compliance for this policy is low. Centralized decontamination requires staff, time, and resources that can be impractical day to day. The project goal is to create a small scale, low cost, quick, and effective disinfectant device to clean respirators, which can be installed right outside of patient rooms all around the hospital, and will allow healthcare workers to easily disinfect respirators between patients, much like the procedure of hand sanitization between patients. The proposed design is a UV-C device that effectively disinfects a respirator in under 3 minutes while maintaining the structural integrity and functionality of the respirator. The team tested the prototype by applying controlled microorganism samples and attempting to decontaminate the respirator with the prototype device. Safety practices and caution considering the various safety hazards coincident with the use of UV-C light were also mitigated via testing. The potential impact of this project is limitless, especially as the pandemic has introduced implications that will continue to stay relevant in the future. This project can help keep healthcare workers and patients safe and improve quality of life.
Team 19: Injection of ethyl-cellulose ethanol to treat refractory warts
Tara Harper, Susan Kang, Darby Welsh, Eric Xu, Sophia Zic
Advisors: Dr. Jenna Mueller and Dr. Melodi Whitley 
Human papillomavirus (HPV) is one of the most commonly transmitted sexual diseases, infecting the skin and creating painful lesions. The HPV virus can remain dormant within the population until surgical transplant or sexual transmission. Previous treatments, such as destructive therapy options, including freezing, surgery, laser and light treatments and salicylic acid, immunotherapy, antiproliferative agents as well as antiviral therapy, for refractory warts are still disputed in their effectiveness and prone to human error; we sought to simplify the treatments without repeated administration. Ethanol ablation is a potential alternative treatment for refractory warts, but suffers from leakage into nearby tissue. Ethyl cellulose (EC), a biocompatible polymer, has been combined with ethanol to reduce leakage and was initially evaluated in an oral tumor model. When injected at a controlled flow rate (of 10 mL/hr), EC-ethanol led to complete regression of oral tumors. Our proposal seeks to develop a single-use, injectable pen that combines and mixes EC and ethanol to inject EC-ethanol into refractory warts. Ideally, the doctor or patient would easily be able to shake the pen to mix the gel solution, with the aid of metal mixing balls, and administer the gel into the HPV wart at a constant injection rate. We found that one mixing ball is optimal for mixing EC-ethanol in our pen device and that magnets can be used to combine and separate the EC and ethanol chambers. We also found that a smaller spring with a smaller plunger than anticipated will eject a volume of liquid. In order to use a larger spring for the desired flow rate, a machine would be needed to compress the spring due to the high force necessary. The simplicity of our design will also make this product distributable and extremely effective in developing countries due to the fact that minimal training, storage and materials are required to operate the injector. The design also has potential in cost effectiveness as the device will operate without the use of electronic components and, while it is made for single use, can possibly be returned to the distributor for refilling and therefore reduce the need for new purchases. Refractory warts have an overall healthcare cost of nearly 300 million dollars and can often lead to psychological burdens due to the stigma of STIs. This device could help eliminate the guilt and blame felt by affected patients by reducing concerns about transmitting infection as well as cutting down on overall healthcare expenses. By effectively treating refractory warts, our design reduces the disfiguring of a patient’s physical appearance and mitigates the spread of additional health risks associated with HPV infection.
Team 20: Simple Compact Monitor to Detect Infiltrated Intravenous Lines
Nathan Alban, Anush Kaovasia, Mariah Jordan, Joseph Manus, Charles Zhang
Advisors: Dr. Ron Samet and Dr. Joe Huang 
With there being such a high percentage of intravenous (IV) injections, there are problems that arise with the catheter on a regular basis. About 16% of IV’s injected become infiltrated - the catheter either pierced the vein all the way through or dislodged after the initial injection. This causes issues for all parties: the doctor/nurse and the patient. Infiltration can cause pain, tenderness, swelling, redness, puffiness, or even hard skin around the IV site, and in extreme cases necrosis of the soft tissue. In addition to this, the medicine is no longer able to be administered through the bloodstream but instead into the soft tissue, potentially resulting in life damaging complications. Without additional technology, it’s difficult for healthcare workers to determine if the catheter is in the vein properly or not. Currently, the admintant flushes the vein with a saline solution to tell if the catheter is sitting in the vein correctly. But because this method is not always visible to the naked eye, they will resort to using an ultrasound probe. While ultrasound machines are effective, they are not always convenient as they require extra parts of equipment (and additional money). As such, we have designed a fluorescent sensor system to determine if an IV is infiltrated or not. By placing the sensor upstream from the IV injection, we have developed a process that uses intravenous indocyanine green (ICG), a laser diode light source to excite the dye, and a photodiode sensor to detect the dye upstream from the insertion. This way, if the photodiode sensor is able to detect the ICG dye upstream of the insertion site and laser diode, there is a confirmation that the catheter is not infiltrated and the patient is able to effectively get their medication. Through our prototype testing phases, we were able to successfully set up a device that emitted a light source to excite the dye through agar gel (simulating skin) and be read by our photodiode detector, in theory. Yet, the values that we obtained from our testing proved to showcase that other factors could have impacted our results as we still obtained a voltage of 5 V, signifying that all of the IR light was picked up (not specifically the light emitted by the ICG). These results could be a result of the reflection caused by the petri dish as well as the potential sensitivity of our current photodiode. The application of our product will provide healthcare workers a simple, low-cost, and effective alternative to a possible life threatening issue that currently exists within the clinical setting. As dominant as the flushing technique currently is, it is not the most effective technique and complications may still persist. With our product, IV infiltration complications that can arise throughout the globe can effectively and efficiently be solved at ease and be deployed in many areas due to our low cost measures.
Team 21: Developing a Powered Air-Purifying Respirator Heads-Up-Display
Sebastian Langan, Alejandro Venable-Croft, Becca Horsley, Jake Morales, and Ian Hidalgo
Advisor: Kevin Aroom
SECOND PLACE 
The goal of this project was to develop a novel technology to improve many clinicians' quality of work. It was determined that this technology must be integrated with the physical environment of a powered air-purifying respirator (PAPR). In the wake of the COVID-19 pandemic, PAPRs have been in increasing use in medical settings to reduce disease spread and other contamination events. Unfortunately, the cumbersome form factor of these respirators makes it a burden for PAPR-wearing clinicians to read and communicate patient vital signs from in-room health monitors. Therefore, there exists a need for a device that can transmit and display patient information such as heart rate, oxygen saturation, and blood pressure into medical professionals' fields of vision while they are wearing a PAPR. Moreover, this device should be able to connect wirelessly with patient monitors as soon as the user enters the room, have a sufficient data refresh rate for real-time patient information, and not compromise patient care due to clinician vision occlusion. Our solution consists of a receiver and transmitter module that communicate via bluetooth. The receiver module is physically connected to a wearable Heads-Up Display headset that would be worn under the PAPR hood. The transmitter module connects to the Datex Ohmeda patient monitor, the health monitor used for this proof-of-concept study. Embedded across the entire design are bluetooth circuits, an RS232-Arduino shield, and Arduino components powered through code. Major prototyping results include drop test deviations for the receiver and transmitter of less than .05 inches from a one meter drop height, and .03 inches for the connector arm. These are both indicators of physical stability of the infrastructure. The other major results were a data refresh rate of 2 Hz related to the OLED display, twice as quick as the initial goal for this value. Furthermore, our solution has a few ethical implications. Through its wireless connection between the patient monitor and Heads-Up-Display, our solution may provide hackers the opportunity to obtain patient health information. Therefore, a more refined version of our technology would need to use sufficient data encryption and related techniques to prevent this type of data leak. However, this design would improve overall healthcare by projecting essential vital signs data in clinicians' field of view, while simultaneously reducing physical stress and discomfort for these medical professionals.
Team 22: The Augmented Reality App for Performing Lumbar Punctures
Eoin Devoy, Moussa Haddad, Kamryn Henderson, George Kotsanos, Talia Morchower
Advisors: Dr. Cha-Min Tang and Dr. Silvina Matysiak
FIRST PLACE 
Lumbar puncture (LP), commonly known as spinal tap, is an invasive procedure used for diagnostic testing and therapeutic effects for neurological diseases.1 When a patient is healthy, and a physician is well trained, a spinal tap is a relatively straightforward procedure with minimal complications. However, the risk for complications and injury increases when a patient is obese, elderly, has other complicating factors like arthritis, or when the physician performing the procedure is inexperienced. There is a need to address complications during lumbar puncture procedures due to physician inexperience and high-risk patients in order to reduce post-procedure complications and procedure time. The combination of augmented reality (AR) and ultrasound (US) technology can be developed to increase the accuracy and ease of a spinal tap procedure. The HoloLens 2 is an AR device that can display holographic information over a real world view, allowing simultaneous visualization of the virtual and physical world. The physician will use the US probe to determine the best needle location and depth, and the HoloLens 2 will spawn a virtual needle in that desired location. The physical needle used to do the LP procedure can then be inserted at the location and depth that the virtual needle is spawned at for accurate needle insertion. In order to design this application we used Unity and Visual Studio design platforms to create a QR tracking app that is able to spawn a virtual needle at a desired location based on the location of an US probe. We used depth dependent QR code detection to determine the optimal QR code size, where 2.9 cm was ultimately selected. Spatial accuracy of the spawned needle was determined by deviation from a fixed point determined by a fabricated testing device. Our results through simulation testing on an artery tissue model illustrated that our app was successful at accurately spawning a virtual needle at the desired location determined by the US probe. From the results we concluded that the app developed has the potential to enhance the LP for the betterment of affected patient populations and enhanced procedural competence of physicians, and warrants further investigation into translation to the clinical setting. QR code tracking capabilities of the HoloLens 2 is a novel and under researched area, making our project a first of its kind. Our project has added more knowledge into the field of QR code tracking capabilities of the HoloLens 2, and its potential use in the medical field.
Team 23: Continuous Oxygen Sensor for Ambu-bag (COS-A): Detection of Oxygen Delivery Errors
Cole Dwiggins, John Abdou, Kate Janos, Brittanni Flores, Jai Dadarwala
Advisors: Dr. Ian White and Dr. Ron Samet 
Ambu-bags are critical resuscitation devices that are commonly used in ambulances and emergency settings to quickly deliver oxygen to a patient. Sometimes, unknowingly, when using self-inflating Ambu-bags, the oxygen supply may be empty, not on properly, or disconnected such that there is diminished oxygen delivered by the Ambu-bag, if any. This can cause panic in an already chaotic emergency scenario. Healthcare professionals may be confused why the patient is responding in an unexpected manner, when the problem is as simple as a flaw in the oxygen supply. We have created an attachment to the Ambu-Bag that reads the oxygen concentration in the air being delivered, and lights a yellow or blue LED based on its measurement. This durable device has no interference with the function and will connect to any standard Ambu-bag. When testing with 100% oxygen, our device was able to detect oxygen concentration differences with a margin of 2% and had a response time of >5 seconds. This provides a fast, simple indication of whether sufficient oxygen is being delivered. Ultimately, the device will make Ambu-bags easier to operate for medical personnel, and therefore safer for patients that require resuscitation.
Team 24: Remote Monitoring of Neurorehabilitation Intervention
Amruth Nagarajan, Arzoo Paracha, Joshua Evans, Nathan Lapinski
Advisors: Dr. Edward Eisenstein and Dr Paola Pergami 
Stroke is a medical condition that affects many people in the world, including 800,000 people in the United States alone. It occurs when there is disruption of blood flow to the brain so it cannot transport oxygen properly. After an individual has a stroke, many side effects can occur including abnormal gait development, which is a cause of losing the ability to walk (Eran Chemerinski). Part of abnormal gait patterns is losing the ability to extend and flex the knee (Tishya A.L.). Rehabilitation from losing one’s ability to walk is a long and tedious process. When the patients are at the rehab facility, they can be monitored by doctors and can make progress on their condition, but once they leave the facility there is potential for regression. Our solution to this problem is a portable device built into a knee sleeve that monitors real-time angular measurements of the knee during the gait cycle. The goal is for it to be able to be worn in a remote environment, away from the rehabilitation facility to increase device accessibility, increase real time data, and limit patient exposure to COVID-19. The data that will be collected will be transferred to the rehabilitation facility to allow doctors to monitor patient progress. Major prototyping results include the knee sleeve device that can accurately measure and track changes in the angle made by the knee during gait while being worn, as well as a MATLAB GUI that is able to produce a knee angle over time graph. Ultimately this device assists in the process of knee gait pattern improvement and proper walking form from heel to toe movement as well as providing remote rehabilitation options for stroke victims. It will allow for shorter rehabilitation periods which will in turn save the patients money and improve their quality of life.
Published May 9, 2022






